Marsha Linehan had a wonderful half-day training on dialectical behavior therapy (DBT) “Where We Were, Where We Are, and Where We Are Going.”
Below are some key take-aways:
* Dialectical Behavior Therapy (DBT) is a treatment that was developed by Marsha Linehan in order to help people with high suicide risk and multiple suicide attempts and/or self-harming behaviors.
-
- The combination of an invalidating environment during childhood plus biological factors are common contributing factors.
- The combination of an invalidating environment during childhood plus biological factors are common contributing factors.
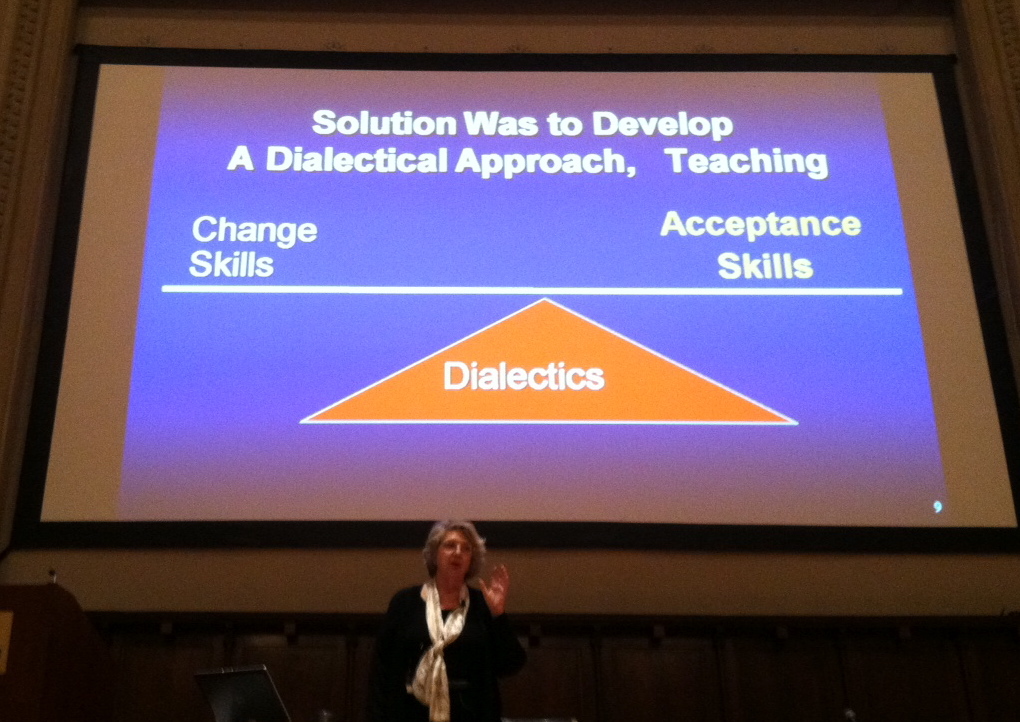
* She developed the dialectical approach balancing both change and radical acceptance strategies to address the fact that the patients with high risk of suicide all exhibited:
- Extreme sensitivity to rejection and invalidation
- making a change-focused treatment unbearable
- Extreme suffering (all clients had suffered extreme traumas in their childhoods)
- making an acceptance based approach also inappropriate
* DBT treatment requires a team; the function of a team is to keep the therapist on track with the DBT protocol.
*Radical acceptance on the therapist’s part entails acceptance of the client’s tragic past, slower rate of improvement vs. other disorders and high risk of suicide/self-harm.
Acceptance is change! Change only happens in the context of acceptance.
*Radical acceptance on the client’s side includes accepting:
- a focus on one set of problems at a time
- the past (what’s past is past)
- the present (some things in the present can also not be changed)
- limitations of the future
* The client is taught radical acceptance skills that include both radical acceptance and distress tolerance skills (to enable the radical acceptance).
* The BPD criterion behaviors (such as the suicidal and self-harm activities) serve as a regulatory function for people with BPD (regulating their emotions) and/or are a natural result of their emotion dysregulation.
| DBT Compared to Expert Community Therapy | ||
| Suicide attempts | 50% | less |
| ER visits for suicidality | 51% | less |
| Inpatient visits for suicidality | 73% | less |
DBT structures treatment goals and targets by level of disorder:
Pre-Treatment: Commitment and Agreement (when treatment first begins)
Decreasing life-threatening behaviors, therapy-interfering behaviors (such as missing sessions or coming late), and quality-of-life interfering behaviors
Increasing behavioral skills: mindfulness, distress tolerance, interpersonal effectiveness, and emotion regulation
Stage I: Severe Behavioral Dyscontrol
Stability and behavioral control (goal)
Stage II: Quiet Desperation
Non-anguished emotional experiencing (goal)
Stage III: Problems in Living/Simple Disorders
Ordinary happiness/unhappiness (goal)
Stage IV: Incompleteness
Freedom and capacity for joy (goal)
DBT added to standard Cognitive Behavioral Therapy (CBT) :
- Model of suicidal behavior
- Acceptance with change
- Integration of evidence-based trainings
- Suicide risk and assessment protocol
- Skills-based on evidence-based trainings and mindfulness skills
- Definition of team as part of therapy
* In general, she stated that the mental health field is moving toward a model in which emotion dysregulation is being considered a core component underlying most disorders. As a result, she thought that it was possible to think that DBT could one day be considered a potential treatment in addressing many mental health disorders (aside from BPD).
* While DBT tends to be viewed as a treatment for people with BPD only, the data indicate that it is already useful for other disorders such as eating disorders and recurrent major depressive disorder.
Where are we going?
- DBT for high risk for suicidal adolescents
- Models for integrating other evidence-based interventions into DBT (Melanie Harned, PhD)
- DBT effects on parenting effects on adolescent suicidality
- Friends and family DBT skills training
- DBT skills as prevention in school systems (Mazza and Mazza)
For the evidence-based training and/or books on DBT, please see Behavioral Tech, LLC.
Finally, below is an excellent video created by the Borderline Personality Disorder Resource Center at NewYork-Presbyterian called “Back From the Edge” which offers guidance on treating Borderline Personality Disorder.
Please note that an interview providing an introduction to dialectical behavior therapy will be coming shortly…
What are your thoughts about dialectical behavior therapy? What are your thoughts about where Marsha Linehan is thinking of taking DBT?
Reference:
Linehan, M., Marsha Linehan on DBT: Where we were, where we are, and where we are going training, May 3, 2012.

Hi Dorlee,
I facilitated DBT skill training groups for 10 years in hospital-based mental health clinics. I agree with the premise that emotional dysregulation is a core component of many disorders. I believe this is often due to insecure attachments in early life that prevent the development of affect tolerance and regulation skills, and/or trauma-induced dysregulation of the nervous system.
I believe this kind of skill-training is essential for clients with these deficits and impairments. However, I believe it is only one component of comprehensive treatment for clients with a history of trauma and impaired attachment. Somatic, affective and relational components are also necessary for the clients to be able to apply the skills when triggered. I have had many clients get frustrated when they know the skills but forget to use them. It takes a lot more work to put it all into practice.
Best wishes,
Andrea
Hi Andrea,
Thanks so much for sharing some of your expertise and knowledge regarding both DBT and treatment of patients with clients with either insecure attachments in early life and/or trauma-induced dysregulation of the nervous system.
I hear what you are saying…that the DBT package would not be a perfect fit for just any disorder involving emotional dysregulation and would require additional techniques and/or modalities.
In all fairness to Dr Linehan, she made the comment about DBT’s application as an interesting observation on her part, not one that she was supporting with research like all the ideas mentioned under the “where we are going now” section.
To avoid any misinterpretation, I will wordsmith that sentence to make sure that I’m relaying that comment as merely an observation on her part.
Thanks again,
Best wishes,
Dorlee