How to Apply Cognitive Behavioral Therapy to Mind-Body Syndrome
Would you like to know how to apply cognitive behavioral therapy to help your clients (and/or yourself) with mind-body pain?
Alan Gordon, LCSW gave a presentation on this very topic at the When Stress Causes Pain: Innovative Treatments for Psychophysiologic Disorders conference and I will be sharing with you some of his key take-aways.
As a brief refresher, many people who are suffering from chronic pain have psycho-psychologic disorders (PPD). PPD cause real physical symptoms that are not due to pathological or structural abnormality and are not explained by diagnostic tests.
PPD manifest as tension headaches, back pain, fibromyalgia, pelvic pain, chronic tendinitis, repetitive stress injury, irritable bowel syndrome, insomnia, chronic fatigue syndrome and more.
Many clients have a hard time accepting that their pain is psychologically-caused and their lack of acceptance is a major barrier to improvement in diagnosis.
It is understandable that we find this diagnosis difficult to accept because the pain is real and it’s a logical conclusion to believe that it is structurally-induced because we take in our information through our senses.
Associated Learning – the process by which an element is learned through association with a pre-occurring element.
For example:
Walking/sitting → back pain
Typing → wrist pain
Running → leg pain
A symptom becomes linked with a particular activity in PPD all the time.
To help a client overcome PPD, reframe the meaning of pain:
• Help client break conditioned response [this can be particularly difficult because the conditioned response may have been reinforced thousands of times; Gordon likens the client’s experience of pain to a kinetic hallucination]
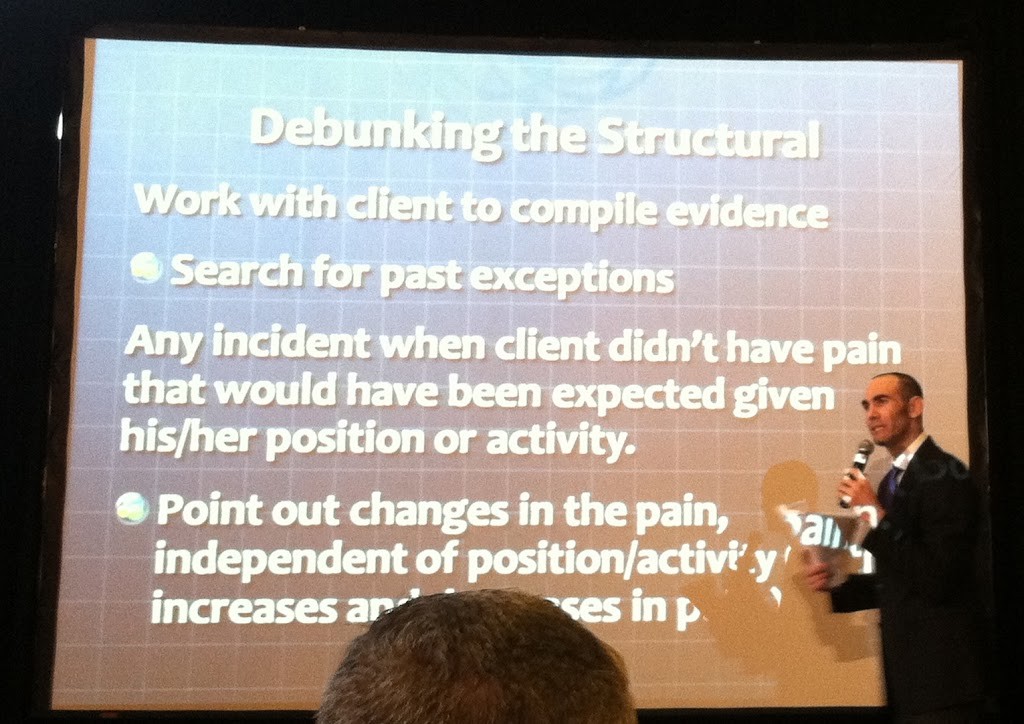
Debunk the structural explanation:
• Help the client come up with counter-evidence; search for exceptions i.e., any incident when the client didn’t have pain that would have been expected given the position and/or activity
• Point out increases/decreases in the level of pain, independent of position or activity (for example, if a client experiences change in pain intensity after expressing some emotion, make note of this)
• Ask the client to put together an evidence sheet to post on in a spot where he/she will see it frequently.
The evidence sheet can have some examples of the counter-evidence listed plus some positive affirmations such as:
“I know it feels like activity/position is causing the pain but the belief that the activity/position is causing the pain is what is actually causing the pain. “
Once the conditioned response is broken, the pain often loses its purpose as a defense mechanism and the client no longer experiences pain.
This is a process that needs to be reinforced over time because there will be relapses and/or pain may appear suddenly in a new area but if you persist, you/your client will ultimately succeed.
Alternatively, you could read and/or visit Unlearn Your Pain by Dr. Howard Schubiner (another presenter at the conference). He has outlined specific steps in his book and/or in his online program that could help you or your clients address chronic pain.
What are your thoughts/comments about the connection between stress and pain?
Like this post? Please share it!
References:
“When Stress Causes Pain: Innovative Treatments for Psychophysiologic Disorders.” NYU Postdoctoral Program and Psychophysiologic Disorders Association, New York, NY, October 6, 2012.

I often notice my pain gets worse when I feel stressed.
When I was dating someone, I often noticed that my neck and shoulder pain was hardly there when I was with her…or rather I was less focused on the pain, however you want to phrase it.
Sometimes I have to tell myself to relax and to relax my shoulders.
Are there sources for this statement: “many people who are suffering from chronic pain have psycho-psychologic disorders (PPD).”? Not to be a pain but I’m genuinely curious.
Thank you for sharing such useful information.
Thank you for sharing your thoughts and questions.
It makes sense that your pain feels worse when you are stressed… this is related to what is called “learned pain pathways,” which can develop after an injury (even a mild one) or can be created during times of significant stress and emotional reactions. This learned pathway gets reactivated in subsequent times of stress.
I will be discussing “learned pain pathways” in my next post in this series.
Sure, one source for the above statement (and for what I just shared about the learned pathways) is:
Schubiner, H. (2012). Emotional awareness for pain. In Rakel, Integrative Medicine, 3rd Edition.
That’s great that you are finding ways to help yourself. Some people also find some solace from chronic pain in 10 to 20 minutes of daily meditation.
Take care,
Dorlee
I have read and used Dr. Schubiner’s book in the past. Interesting and enlightening but not useful in the long run. Now in EMDR treatment that is evidence-based and offers a better chance of resolving issues that lead to pain.
Hi Lesa,
Thanks so much for stopping by and sharing your experiences. I’m sorry to hear that CBT and/or Dr Schubiner’s approach to pain management hasn’t been of much help to you but so happy to hear that you are finding EMDR beneficial.
Best,
Dorlee