What are some of the evidence-based practices for trauma-informed care? Have you wanted to learn more about narrative exposure therapy?
A few weeks ago, NYU’s Silver School of Social Work held an informative one day conference on the “Core Principles of Trauma-Informed Care: The Essentials.” In part one of this series, you had the opportunity to look at what is the essence of trauma-informed care.
There are many evidence-based treatments for trauma such as EMDR, yoga, drama therapy, improvisation, movement therapy and rhythmic singing, but this post, part two of the series, will be focusing on narrative exposure therapy.
Below are some key take-aways for you vis a vis evidence-based practices for trauma, as per Carol Tosone, Ph.D. and Associate Professor at the Silver School of Social Work,
Evidence-Based Practices for Trauma
Before delving into effective trauma treatments, Tosone first reviewed Psychological First Aid (PFA) and shared a wonderful grounding exercise.
Principles of Psychological First Aid (PFA) include:
- Safety – developing/identifying a physically safe environment
- Efficacy – maximizing an individual’s ability to care for self, family and others
- Calmness – teaching and encouraging relaxation and calming skills (as well as maintenance of natural body rhythms such as sleep, food, exercise)
- Connectedness – facilitating links to family and other social supports
- Fostering Hope and Optimism
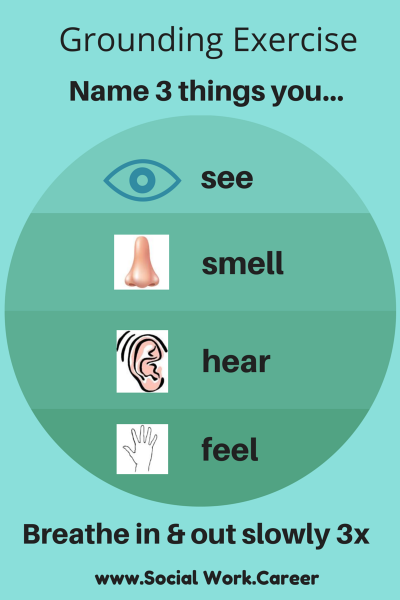
Grounding Exercise
To help your client feel grounded, ask her/him to:
Name 3 things you see.
Breathe in and out slowly three times.
Name 3 things you smell.
Breathe in and out slowly three times.
Name 3 things you hear.
Breathe in and out slowly three times.
Name 3 things you touch/feel.
Breathe in and out slowly three times.
This grounding exercise [free download] is also helpful for calming or relaxing purposes. If you struggle with panic attacks, you may also wish to check out this post with additional grounding exercises (and a free download).
Effective Trauma Treatments (van der Kolk) include:
- Eye Movement Desensitization and Reprocessing (EMDR)
- Yoga
- Drama Therapy
- Improvisation
- Movement Therapy
- Rhythmic Singing
Narrative Exposure Therapy (NET) (Weisel, 1996)
The client or survivor typically:
- Wants and needs to communicate but at the same time terror is speechless (both needs coexist)
- Feels misunderstood
- Experiences physiological alarm state during event and feels helpless/terrified
- Doesn’t want to contaminate others, wants to protect others
NET’s Cultural Flexibility (i.e., can be employed with any population anywhere)
- Story-telling, oral tradition and verbal expression are shared among all people
- It has been demonstrated to be effective under a variety of conditions from refugee camps to outpatient settings
- It allows for reflection of one’s life in its entirety – People naturally try to heal themselves through the narrative, through the process of habituation, you learn to overcome it. You contextualize it, you reconstruct it.
- It is suited for Type II trauma – When they’re too engaged, you bring them back. You need to help people go through it in a palliative way.
- Treatment of members of traumatized societies is necessary to break the cycle of violence and trauma, as well as foster forgiveness and reconciliation.
NET Targets Symptoms of Complex Post Traumatic Stress Disorder (PTSD)
This includes somatization as well as changes in:
- Regulation of affect, impulses, attention or consciousness
- Self-perception
- Perception of the perpetrator(s)
- Relations with others
- Systems of meaning
Narrative Exposure Therapy Process/Procedure
- Approx. 10 sessions of 90-120 minutes
Session 1
- The person constructs a detailed narrative of his/her biography and the therapist writes down the testimony – at this stage, you’re not engaging the hot memories; you’re just documenting them.
- Assessment (demos, medical and psychiatric hx, current complaints) and evaluation of PTSD
- Psychoeducation – normalization, description of trauma reactions, explanation of the therapeutic procedure
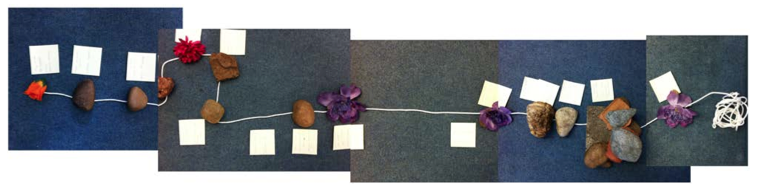
Lifeline Illustration: Flowers represent positive life events and stones symbolize traumas
Session 2: Lifeline
- This is a visual and symbolic representation of the person’s life story to show survivor that his/her life is so much more than the trauma(s).
- Survivor places positive and negative life events in the form of flowers (positive) and stones (negative) in a row (formed by a rope or string etc) in chronological order.
- Therapist guides person in the process of laying these symbols while classifying them; therapist stays on cool-memory side and does not mix imaginative exposure elements into this session.
- This exercise is completed in one session.
- KIDNET for children; lifeline is laid out each time as a beginning exercise.
- For adults, a photo of the lifeline is available at subsequent sessions to orient the person to period being narrated, as well as what has been discussed & remaining work to be completed.
Session 3: Start of Narration: Birth -> First Traumatic Event
- Chronological facts + emotional processing of events – trauma is timeless; it gets embedded in our memory
- When the first traumatic event occurs, person may become nervous. Allow sufficient time (40-60 mins).
- Contextualize the traumatic event:
- Time and setting
- Location and activity (where and what person was doing at the time)
- Beginning of incident is marked
- Narration shifts to SLOW MOTION and person is instructed to imagine the beginning of the incident, focusing on perceptions during the trauma (physical sensations, thoughts, actions, shapes of objects, smells, sounds)
- GROUND PERSON in PRESENT– person is in present time discussing past events (to avoid dissociation and flashbacks).
- HOT MEMORY – is activated and elements of fear/trauma structure are put into words/narration.
- HABITUATION –You decrease symptoms after exposure to memory.
- Continuous process of activating & narrating hot memory > decreased emotional & physiological arousal over time
- Session should not be stopped until some degree of habituation has taken place (if person is left at peak arousal, symptoms have been aggravated).
- HOT memory is transformed to cool memory (decreased physiological and emotional reactions)
- Help person verbalize what happened following incident: When did it end? What were you doing? Who were you with?
Session 4 and Subsequent Sessions
- Rereading of narrative and continuation of narration of subsequent life events
- During last session:
- Testimony should no longer have its arousing impact (i.e., it should be recalled with some sense of emotional distance).
- As in the beginning, survivor’s lifeline is symbolically presented via stones and flowers in chronological order.
- The closing ritual is to focus on the testimony, inclusive of survivor’s entire biography, with emphasis on the courage he/she had to face the trauma in its entirety and in the context of his/her whole life.
- Many people move on to forgiveness and advocacy.
Eye Movement Desensitization and Reprocessing (EMDR)
EMDR is another evidence-based practice for trauma. It was developed by Francine Shapiro in 1989 as an 8 stage treatment for Post-Traumatic Stress Disorder (PTSD).
Below is a 7 minute video clip that gives a good illustration of an EMDR therapy session.
EMDR entails:
- History, Treatment Planning and Client Preparation
- Processing
- Assessment of Trauma-Relevant Target(s)
- Desensitization and Reprocessing
- Installation of Alternative Positive Cognitions
- Body Scan for Continuing Discomfort or Trouble Spots
- Closure (addressing constructive coping needs for client’s future use)
- Reevaluation
To find out more about this technique, please make to check out the informative interview with Andrea Goldberg, LCSW What is Eye Movement Desensitization and Reprocessing (EMDR)?
What example could you share of when you have employed one of the above described techniques (PFA, NET or EMDR)? And/or what is one valuable learning you reaped from your experience?
Please share your thoughts below.



[…] SOCIAL WORK CAREER. (2014). Core Principles of Trauma Informed Care Key Learnings. Grounding Exercise. Recuperado de: https://www.socialwork.career/2014/07/core-principles-of-trauma-informed-care-key-learnings-2-of-3-ht… […]