The Neurobiology of Trauma
Have you wondered how trauma impacts the brain and body? Or what you might do to help counteract its effects? Judith P. Siegel, Ph.D., LCSW, Associate Professor at NYU’s Silver School of Social Work gave an informative presentation about the neurobiology of trauma and the whole mind/body connection.
This post will provide you with some of the take-aways from Siegel’s talk.
- Trauma can change your brain and alter your cells. When your body cannot process trauma, it gets expressed via your body.
For those of you who missed the earlier posts of this series based upon the conference NYU’s Silver School of Social Work held on the “Core Principles of Trauma-Informed Care: The Essentials,” part one of the series addressed the Principles of Trauma-Informed Care and part two reviewed evidence-based practices for trauma-informed care, particularly narrative exposure therapy.
- Brain stem
- Hippocampus
- Amygdala
- Frontal cortex
- Freeze/flight or fight [hyperarousal response]
- Detachment or numbness [dissociative response]
We are wired to respond to perceived dangers. Our beliefs and expectations which are influenced by our past trauma(s) either reinforce or eradicate the conclusion of danger.
In a state of heightened arousal, the left and right side of the brain disconnect.
There Are 2 Types of Dysregulated States:
- Exploder – rage reaction; externalizing, a moment of overreaction
- Imploder – holding in emotions; internalizing
OR
- SHUT DOWN – the ultimate surrender and statement of helplessness [this often goes unnoticed!] – similar to the affectless states described by Bowlby in his research (1959) with infants and young children exposed to extreme loss.
- the ability to “know” several aspects of self experience at any given time
- being able to recognize physical sensations, feelings and thoughts (as well as activated memories that contribute to the experience)
- In the experience of trauma, what you saw, felt, smelled… there were different parts of the brain involved. Neural (memory) networks contain and connect them all.
- Neural networks connect:
- Physical, emotional and logical aspects of self
- Past and present
- Many areas of the brain
- Appraisal with experience
- You make sense of the present based upon the past. When one aspect of your memory is triggered, all aspects are activated, including past emotions.
- Revived memories inform cognitive functions such as making judgments, drawing conclusions or impacting your expectations. They also tend to flood the present.
- When/if find yourself having a very strong (over) reaction to a present event, consider:
- Is it possible that your current response is including some reactions/feelings from the past?
PTSD (Post Traumatic Stress Disorder) – when a person is experiencing PTSD, the fear circuitry is no longer being integrated with the executive centers of the brain located in the prefrontal cortex.
As a result, individuals with PTSD may experience “fight” or “flight” responses from relatively minor stresses. These, in turn, lead to increased heart rate, sweating, rapid breathing, tremors and other symptoms of hyperarousal.
As a result of trauma, the sense of being out of control which is associated with the helplessness an individual had experienced could you put him/her in a state of dysregulation.
How to Help Clients Repair Their Brains?
- Strengthen the Family – the family can provide a sense of stability, hope and connection. It can provide secure attachment. Strong families have a sense of safety and an expectation of successfully managing problems and stressors.
Children who have been through trauma but have protective and loving parents do well.
- Build Emotional Regulation – helping individuals increase their capacity for self-awareness, tolerance, comprehension and thoughtful responses; helping them become aware of their emotional and physical states, being able to acknowledge and sit with their feelings without becoming overly anxious.
When You Feel Stress, Pay Attention to Your Body:
- What are you feeling?
- Where are you feeling?
Your body is trying to inform you…
Examples of How You May Feel Under Stress:
- Numb, nauseous, tense, tight, light, clammy, faint, shaky, jumbled, dense, warm, cold, tingling, fuzzy, clear, sweaty
- Tightness in neck, shoulders, stomach, gut, back…
- Head is swirling, empty, darting from thought to thought…
How to Improve Emotional Regulation?
- Breathe – see breathing exercise for description and easy to remember graphic
- Mindfulness – enables you to:
- Perceive feelings without reacting to them
- Be nonjudgmental of your own experience
- stay present with perceptions, sensations, thoughts or feelings (even when unpleasant)
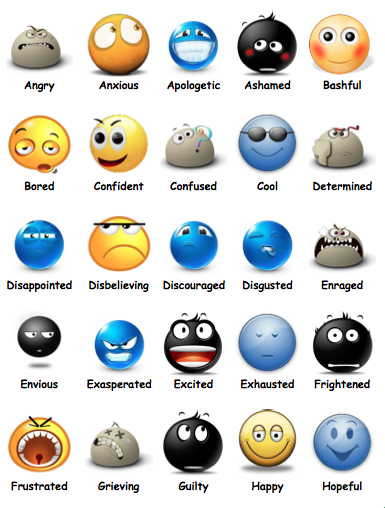
- Naming feelings – this is another technique to impact the neural networks in a positive manner. The neural network is essentially activated to figure out the emotion.
Studies have shown that when individuals are shown emotional images and asked to choose between two words to describe it, changes take place in the brain.
There is an increase in the symbolic processing of emotional information and a decrease in activity in the amygdala, linked to processing memory and emotions, along with the “flight or fight” fear response.
In other words, simply naming an emotion helps disrupt emotional responses in the brain.
Next time you are experiencing an unpleasant feeling, name it. Use as many words as you feel you need. Using a list or chart of feeling words such as the one shown above may be helpful.
Integration
With integration, individuals are able to connect in a thoughtful way:
Emotional Response + Trigger + Memories > Acceptance
You want to help the client understand his/her trigger and bring the memory back, but this time, you are going to help change the memory network so that when it gets reintegrated, it won’t look the same. The client will either take something out or add something new. You’re not just going to talk about it with the client. (That would almost be a waste of time.)
In a Dysregulated State…
“It is important to remember that verbal interpretations processed by the left hemisphere are not going to access the right brain.” – Alan Schore
Many people become advocates after trauma – this is not coincidental; it is the result of how they have found meaning in their trauma.
Guided Imagery Finale
Siegel concluded her presentation with a pleasant guided imagery exercise. It was a very enjoyable way to have a talk end. Briefly, she suggested that you take an image of when you’re feeling good and truly notice what it smell likes, looks like and sounds like.
Then when you’re under stress, this is an image that you would be able to access by bringing it back up for yourself, looking once again at the image and re-experiencing in your imagination all the ways in which you felt good… this will then bring back for you all those good feelings in your brain and body!
This post brings us to the end of the series based upon NYU’s 2014 trauma-informed care conference. I hope that you found some of this information useful.
What are your thoughts/comments? How helpful have you found increasing emotional regulation in your trauma work with clients? I’d love to hear from you 🙂
Like this content? Sign up for more posts like these !
Image Attribution:
Emotions from My Feelings Workbook
Trauma Informed care image/definition

Thank you very much Dorlee, for another terrific and very helpful edition of the Social Work Career Development Blog!!!
Sincerely,
Ernest Wahrburg, MSW, LCSW.
Thanks so much, Ernest, for your very kind feedback 🙂
Best,
Dorlee