21 Dementia Tips for Caregivers and Social Workers
Do you have a relative or clients who are wrestling with dementia, and would like to find a way to either help or better connect with them?
Thanks to the generosity of Dr. George Huba, this post will provide you with 21 invaluable tips:
- 7 Ways to better cope with cognitive impairment
- 7 Ideas to improve your ability to care, connect and empower your relative or clients
- 7 Areas to advocate on behalf of those with neurodegeneration to improve their quality of life
As some of you know, Dr. Huba is a psychologist who has over 35 years of experience working as a high tech scientist working in the evaluation of social and mental health programs for the poor, as well as methods for psychological test development.
While he was diagnosed with a neurodegenerative disorder seven years ago, he serves as an inspiring example of someone who is trying to use all the tools and knowledge he can find to maintain the best quality of life possible, and help others at the same time!
Dr. Huba is able to fight back his cognitive decline via the use of mind mapping and a few additional tools and techniques. He blogs and has even written a book on this very topic Mind Mapping, Cognitive Impairment, and Dementia [affiliate link].
As you will see from the below samples of the wonderful mind maps that he uses to express himself, you cannot help but take your hat off to him for his wisdom, courage, strength, and determination to do his utmost with the available tools so as to lead the highest quality of life possible.
So without further ado, George, could you give us a bit of your background?
I was diagnosed with neurodegenerative disorder in late 2009 at the age of 58. I had fallen walking out of a football game at the University of North Carolina and shattered my left shoulder blade so completely that it took 20 pieces of surgical metal and two operations to repair.
I had been in treatment with a psychiatrist for several years with bipolar disorder being the diagnosis before receiving the neurologic diagnosis which covered many of the same symptom patterns. I retired in late 2011 after my neurologist and I concluded I could no longer do my job (evaluating psychosocial and medical programs) well and I felt my own judgment would be questioned were I to continue to work.
The Social Security Agency – through a new and special program called “Compassionate Allowance” – had their doctor confirm the diagnoses of several neurologists I had seen, and determined that I had one of the conditions which, without question, is seen as fully disabling. Any social worker not familiar with this program should look at the web site of the US Social Security Agency to learn about this important and innovative program.
What made you think about making mind maps to assist you with your dementia and how they have been of help?
I had been making the equivalent of mind maps and concept maps since my undergraduate years in the early 1970s and continued through my career, although these semi-common diagrams among psychometricians such as myself were called path diagrams, structural equation models, hierarchical factor structures and other names.
They were really all mind and concept maps without a few of the artistic features now common such as color, bright images, and fancy fonts. My published computer program in the late 1970s has been identified as the first automated program for producing such diagrams, and although not called a concept or mind map program did produce diagrams that were functionally similar.
Throughout the period 2005 through 2010, I had watched my verbal skills decline as my memory (especially immediate recall) and other cognitive functions changed. I had been using modern mind mapping methods and programs since the early 1990s. I was fairly quick to recognize in 2010 that while my ability to speak and write was becoming “disabled,” it seemed that I could diagram and remember and reason through diagrams far better than I could through words.
I discuss on Hubaisms.com (my blog) the positive outcomes this had on my daily quality of life (I believe I am a “Person Living WELL with Dementia), as well as how far I am willing as a scientist to generalize my experience to others.
Would you recommend a particular mind mapping program versus another (and if so, what are its advantages and disadvantages)?
I have reviewed mind map programs about annually on my blog. I discuss programs for the Mac (most also available in identical form on the PC), iPad, and iPhone. Many of the comparative features are discussed in detail.
I have always concluded – ever since I started – that the program iMindMap (created by a team headed by Chris Griffiths) is far superior to any other program. I recommend that social workers and other professionals (and just about anyone else) learn and use this program. While the program will seem a little strange in the first hour, there are probably 20 hours of free video training modules on the Internet on the iMindMap.com site. After the first 3-4 hours a social worker could produce a good mind map useful with a client and other social workers.
The disadvantage of iMindMap is that it is among the higher priced of the mind mapping programs, although by no means the most expensive. One should purchase the Ultimate version. You will – within a month or two – be using the advanced features. Historically the program has cost several hundred dollars and annual updates (usually very impressive) are offered at a fraction of the initial cost.
Let me emphasize that there are dozens of “free” mind map programs and other “advanced” programs selling in the range of $5-$30. Compared to these alternatives, the price of iMindMap seems quite low. It is the best, it is “expensive,” it is worth it, and it can be a true professional tool in the hands of a social worker or other similarly-trained individual.
Out of all the mind maps that you’ve created, which are the best ones for a person with dementia to consider using ?
This is an extremely difficult question for me to answer. There are 580 posts on my blog which started in 2012 including 1000s of mind maps. Interestingly, as part of my dementia I can only remember the last one or two I developed, and I have to go back and look at my list every time I start working on them to make sure I am not being redundant. I knew that I would have to deal with this issue both for myself and users. So, on every page near the top left there is a search box. This will recover all of the posts for such search topics as “social work” or “caregiver” or “financial” or “self esteem.”
You can easily find 5 or more posts on hundreds of issues. So my answer would be “the most recent five on the topic I was interested in at the time.” The site was intentionally designed to work like that for a person with dementia – me – who cannot remember the details of his own work, often from a period of a few minutes or a few hours earlier.
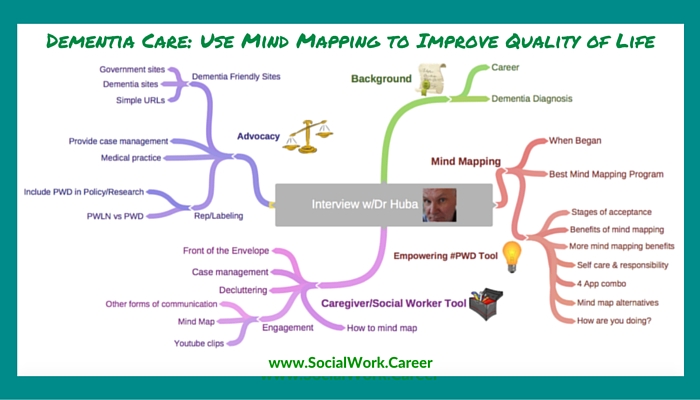
Looking through Dr. Huba’s vast collection of posts, below are the mind maps that I thought may be most useful. To see a larger view of each mind map as well as Dr. Huba’s descriptive text, click on the map images.
7 Great Mind Maps for People with Dementia
The Necessary Transition to Live Better with #Dementia
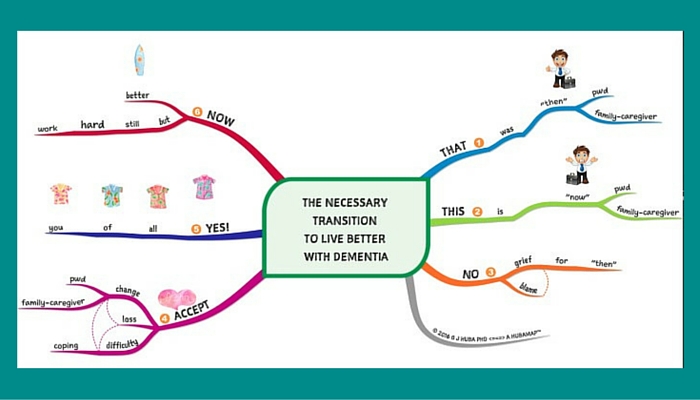 This mind map illustrates the stages of acceptance people with cognitive decline (and their caregivers) go through. Not surprisingly, the sooner one accepts the reality and using coping various cognitive behavioral methods, the easier it is on both the PWDs (persons with dementia) and their caregivers.
This mind map illustrates the stages of acceptance people with cognitive decline (and their caregivers) go through. Not surprisingly, the sooner one accepts the reality and using coping various cognitive behavioral methods, the easier it is on both the PWDs (persons with dementia) and their caregivers.
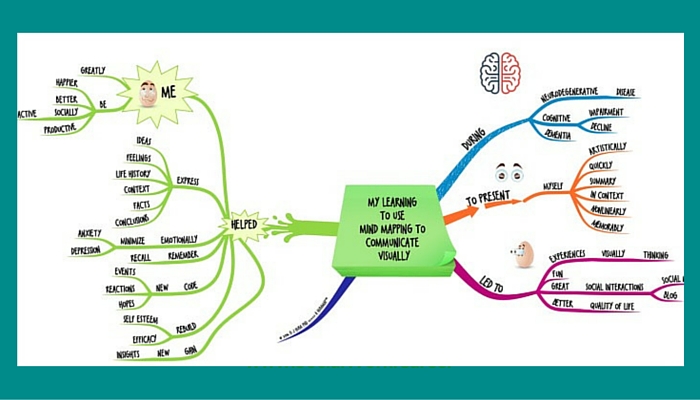
What Happened When I Learned to Use #MindMapping to Communicate Visually?
This graphic illustrates how mind mapping may empower individuals with dementia by enabling them to express themselves, be more productive and feel better emotionally and mentally.
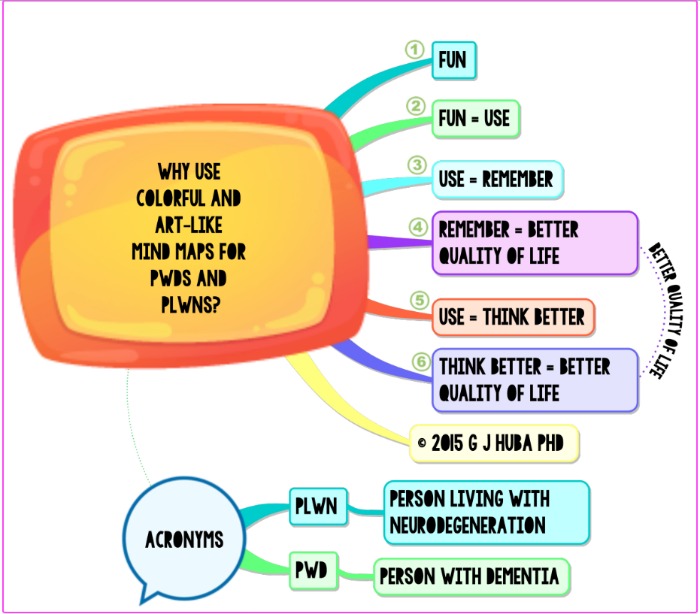
Why I Endorse the Stylistic Use of Bright and Art-Like #MindMaps for Persons with #Dementia
This mind map sums up the main reasons why it pays for individuals with cognitive decline to engage with mind mapping. It is fun; it helps them think and remember better and thus improves their quality of life.
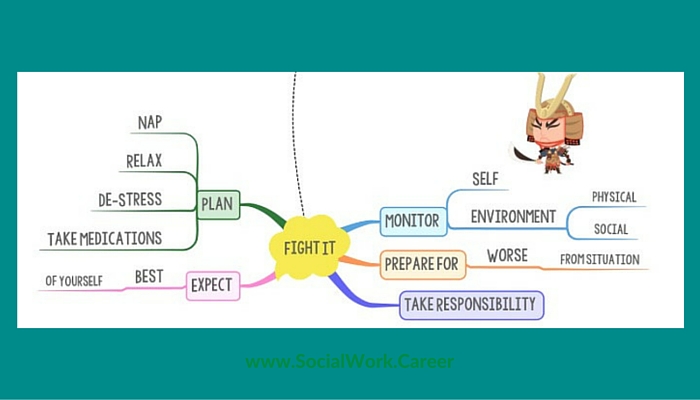
Don’t Be a Jerk with #Dementia [click on link to see full map]
This mind map serves as an excellent reminder for those who have cognitive decline to engage in self-care and take responsibility for how they feel. When people with dementia get sufficient rest, naps and take their medications as recommended, they will feel and behave at their best.
4 “Live Well with Dementia” Apps – this mind map lists the four apps that Dr. Huba uses to handle all his daily thinking tasks (tools that may benefit anyone): google (for finding information), Snagit (for clipping parts of information into different formats), Evernote (for storing information) and iMindMap (mind mapping).
Secondary Alternatives to #Buzan #MindMaps for People with #Dementia or #CognitiveImpairment – Out of the eight alternatives to mind mapping that Dr. Huba has tried and evaluated, he found three that may work well as alternatives to mind mapping: Sketch Noting by Mike Rohde, Doodling by Sunni Brown, and Cartooning by The Oatmeal.
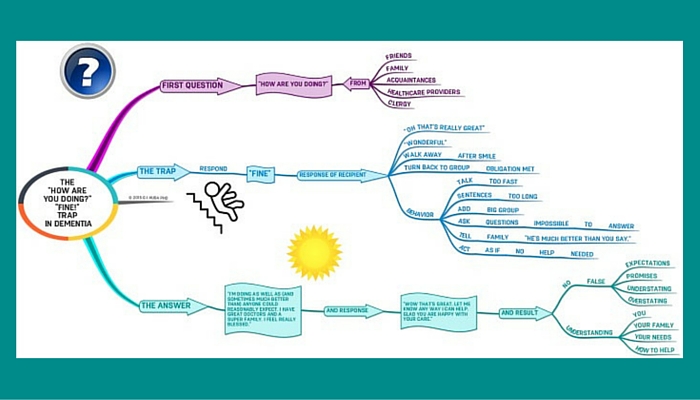
The “How are You Doing?” “Fine!” Trap in #Dementia
This graphic illustrates how best to respond to the question “how you are doing” and why. Saying you’re “fine” is not the way to go as Dr. Huba so cleverly illustrates!
And which of your mindmaps are best for the caregiver (or social worker) caring or working with the person with dementia?
Looking through Dr. Huba’s huge collection, below are the mind maps that I thought may be most useful for caregivers or social workers. To see a larger view of each mind map as well as Dr. Huba’s descriptive text, click on the map images.
7 Great Mind Maps for Caregivers/Social Workers
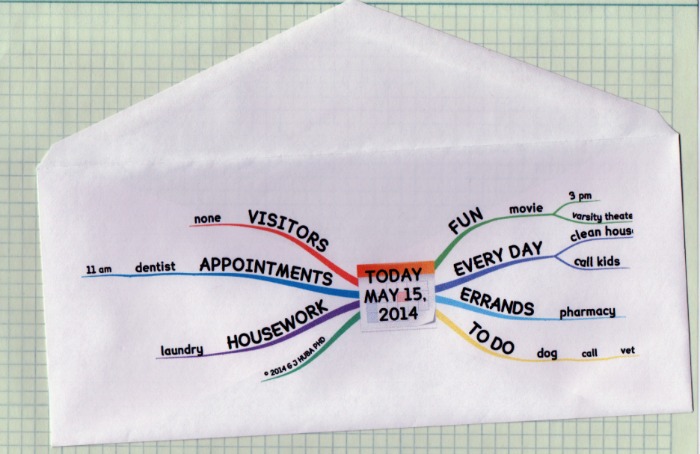
Front of the envelope planning
The caregiver (or social worker) may create a schedule for the person with dementia using a mini mind map on the front of a standard business envelope (#10). The envelope serves double duty as both the daily planner and container for any receipts, prescriptions received from the doctor etc. throughout the day. This type of planning tool is both more engaging and easier for a person with cognitive decline to use/remember than a standard list.
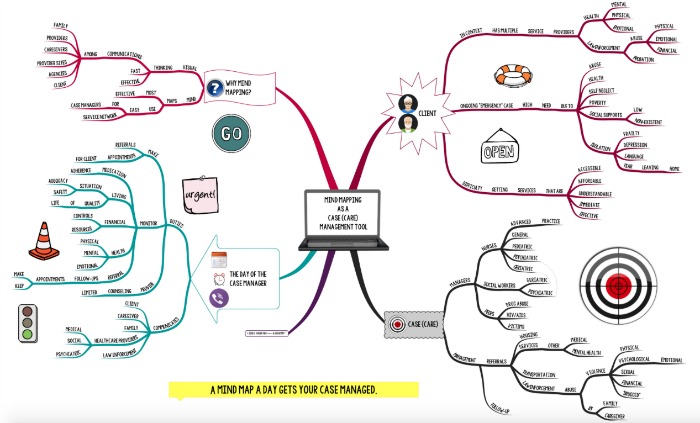
http://hubaisms.com/2015/11/03/mindmapping-is-a-powerful-tool-for-nursing-socialwork-and-peer-casemanagement/?
This graphic illustrates how mind mapping may be used as a case management tool.
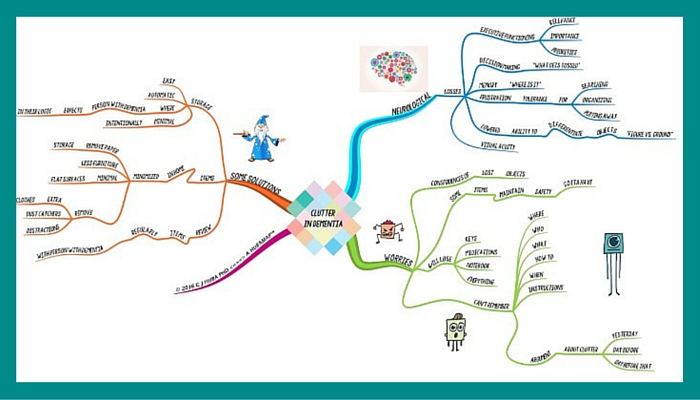
#Dementia and Decluttering: Clean Up Ideas for Persons with Dementia and Caregivers
This graphic explains some of the reasons individuals with cognitive decline may struggle maintaining order with their belongings and provides some suggestions on how caregivers may assist in this area.
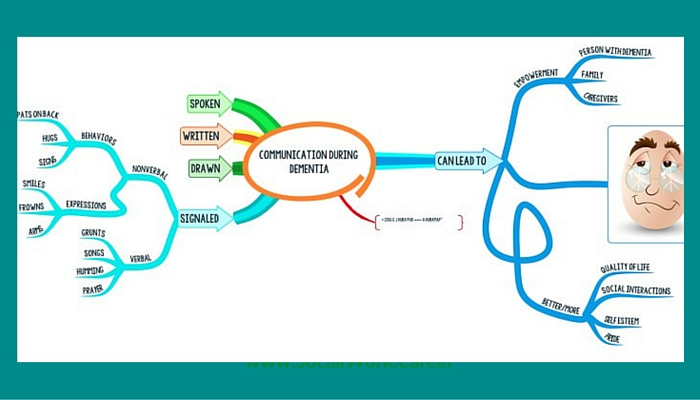
Communication During #Dementia
This graphic illustrates the importance of communication to individuals with cognitive decline as well as some of the alternative ways that one may communicate other than words. It is worthwhile communicating via drawing and signaling because talking may be the least effective way of reaching a person with dementia.
A Simple Way to Engage a Person with #Dementia #PWD to Understand #MindMapping as a Way to Communicate – this post provides a mind map of possible topics that you can use to converse with dementia, as well as a link to videos of Dr Huba demonstrating the process of creating a mind map.
Once you select your topic, it is recommended that you create a simple mind map of the questions you’d like to ask your person with dementia so as to give it to your PWD. This will help your PWD be able to talk with you because they will have something in their hand to remember what you are asking/talking about.
At a Loss About Starting a Conversation with a Person with Dementia? – this mind map includes another list of possible topics that you could use to talk about with your person with dementia; however, it is tailored to using a 3 minute youtube clip as the conversation starter (and you would then follow up with a few questions about the clip via a mind map).
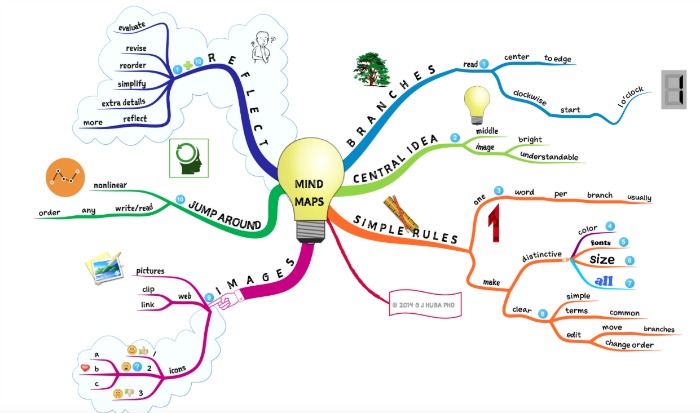
How to Mind Map: Demonstration of Text vs #MindMaps in Instruction
This mind map details the steps of mind mapping.
Are there other tools that you recommend caregivers/social workers use to engage with individuals with dementia?
The most important methods I talk about in the blog are “doodling” to store and share memories and also to make one focused and calm, and a very nice method developed by Mike Rohde called “sketchnoting” or “sketchnotes.”
There are dozens of posts on these two methods and why they are important in the blog.
Do you find having dementia scary? Or do the mindmapping tools enable you to address much of the memory problems and thus make dementia feel like a manageable illness?
My most recent blog post (on dementia being a wild roller coaster ride) was written yesterday. Yes, it is terrifying at times but mostly manageable. The terrifying part is that I know it will get worse. The most scary part for me is the impact that the condition has on others now and in the future, and not that it has on me.
I often argue in posts that in the absence of proven medical treatment methods, the best way to deal with cognitive impairment and dementia (as well as typical decline with aging) is through inexpensive behavior and cognitive tools. I have tried many. Mind mapping works best for me.
I strongly urge other individuals to study art therapy which shares many features with the methods I use. My belief is that studying art therapy and mind mapping would perhaps permit us to begin cognitive interventions by combining the well researched area of art therapy with mind mapping and sketchnoting.
How may caregivers and/or social workers become more attuned and sensitive to the needs of those with dementia?
Look at my blog for lot of posts on surprising things that unaffected people do not recognize about dementia. For instance, the fact I cannot recall your name or if I took a pill two hours ago does not mean I cannot recall what I read and some of my term papers from college or high level mathematical equations from my career at the same time as I cannot do a third-grade word problem.
It feels to me like the brain is Swiss cheese. Lots still there but there are some holes in completely random places. A good picture is the Cheese-heads who root for the Green Bay packers.
Social workers MUST realize that dementia is not a disease. Rather it is a cluster of symptoms that result from different types of brain diseases, chemical imbalances, and trauma. Dementia does not equal Alzheimer’s disease which I do not have. Dementia need not include memory loss for many, especially until it reaches very advanced stages. Dementia may also be a secondary diagnosis for those primarily diagnosed with having another condition (a good example is Parkinson’s disease).
Looking through Dr Huba’s blog, below are the top advocacy related mind maps/posts that stood out to me. To see a larger view of each mind map as well as Dr. Huba’s descriptive text, click on the map images.
7 Great Mind Maps/Posts Calling Out for Cognitive Decline Advocacy/Cultural Sensitivity
Friendlier Websites/URLs
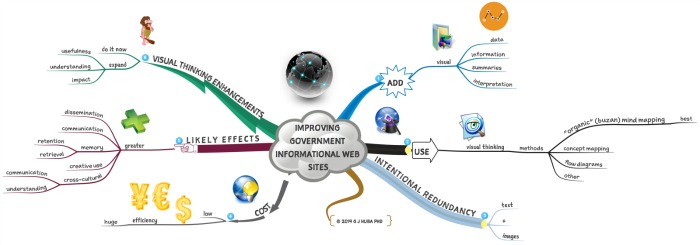
Increasing the Usefulness of Government-Supported Informational Web Pages at Almost No Cost
This mind map is asking for governments to start producing their information in a more visual-friendly format (mind map, flow-chart or concept map) to make the information more easily digestible by those who have difficulty with the English language, are more visually-inclined or are suffering from cognitive decline.
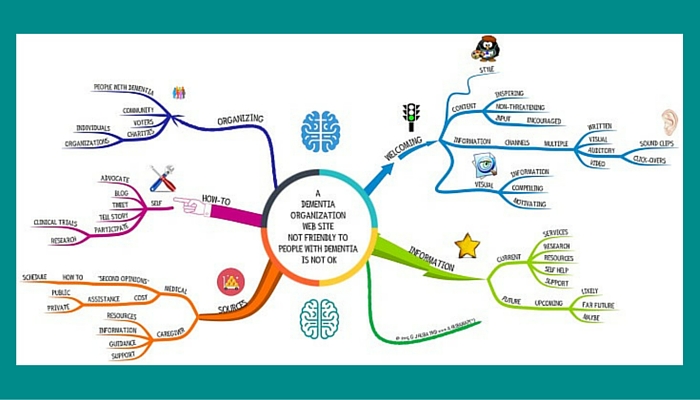
#Dementia Web Sites Not Friendly to People with #Dementia Are Not OK
Sadly, dementia websites do not seem to be any better than governmental ones. This graphic is crying out for all the sites catering to those with dementia to make their sites dementia-user friendly! Currently, the vast majority of information is not relayed in ways that would be accessible to people who are with cognitive decline. If the information were relayed visually via mind maps, concept maps or flow charts, more dementia users would be able to benefit from the content dementia sites are providing.
Stoopid #FBI and #AARP Internet Tricks Undermine Excellent Elder Abuse Scam Prevention Information – in this post, Dr. Huba recommends that governmental sites employ short URLs so as to make it easy for the elderly and those with cognitive decline to reach out for help.
Case Management/Medical Practices
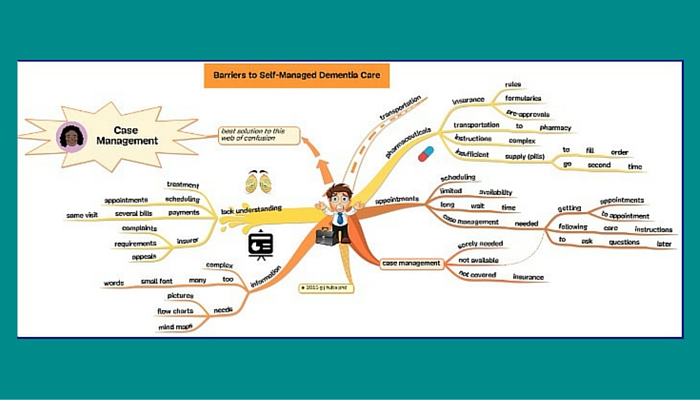
#Barriers to Self-Managed #Dementia Care
This graphic shows how the barriers to self-managed dementia care include too much [complex] information, scheduling of appointments, handling of insurance claims, transportation issues and more. However, outside insurance covered case management could facilitate self-managed care!
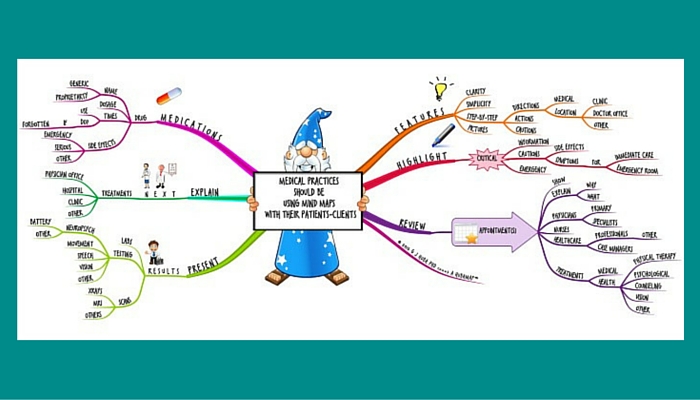
Medical Practices Should Be Using #MindMaps with Their Patients
Dr. Huba demonstrates the various ways that offices could provide their information to their patients via mind maps such as the medications (names, dosages, times), treatment information, results of tests, appointments and the greater patient engagement and compliance benefits that would result from medical facilities taking this type of action.
Representation/Labeling
Where are the Consumer (People Living with Dementia) Representatives in Dementia Public-Professional Policy and Research Initiatives? – post in which Dr. Huba raises the important point that individuals with dementia are being left out of the important conversations such as the one being conducted by the American Academy of Neurology and the American Psychiatric Association regarding a process in which they developed draft consensus measures of Dementia Quality.
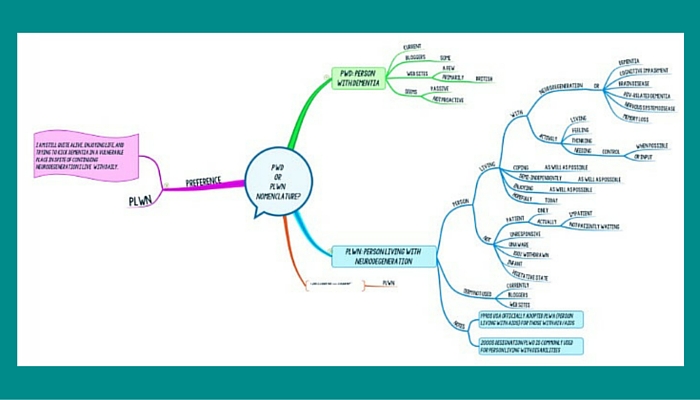
This mind map shows quite powerfully how the labels one uses for different conditions matter. A person with dementia (PWD) is typically viewed as rather passive and not proactive. This is in marked contrast with the term a person living with neurodegeneration (PLWN) who has so many other possible states of being and coping including coping as well as possible, living semi-independently, feeling, thinking, and controlling/providing input when possible.
Dr. Huba views himself as the more fitting and empowering term, PLWN and living well!, and would like the professionals in the field to start using this term!
Is there anything that you’d like to add?
Let me note that I try to answer any question – if I can do so – which is made in response to one of the posts in the blog. I won’t always know the answer and I won’t always be able to interpret the question and sometimes I won’t remember to check for new comments every day, but I do try to answer the questions as soon as I see them.
Please also follow my Twitter @DrHubaEvaluator. It lists every time there is a new post on my blog and provides a direct link.
In response to some of the questions/comments that have come through below (as well as on twitter), I’d like to share a link to a short video clip which illustrates the important role that google plays in maintaining my independence.
Note that with the exception of the first mind map created by SocialWork.Career, all of the above mind maps are Dr. Huba’s creations © G J Huba PhD and are shown here with his express permission.
Thank you, George, for being so courageous and giving with your expertise!
As a reminder, Dr. Huba has authored Mind Mapping, Cognitive Impairment, and Dementia [affiliate link] with hundreds of mind maps providing additional guidance about how to improve the lives of individuals with cognitive impairment.
Like this post? Please share it!

Thank you so much for posting this. I have worked with people living with dementia for many years and looked at (and used) graphics but never even considered the use of mind maps in this way but can see already many very practical implementations. It’s great to see the examples and I feel sure this post will be incredibly useful and inspiring for many – colours and logical visual representations can be used in many ways to help clarify.
Thanks so much, Ermintrude, for your kind and thoughtful feedback on my interview with Dr. Huba!
I’m so glad that this post has been instrumental in showing you practical applications of mind mapping with people living with dementia 🙂
Thanks again,
Dorlee
Thank you for your comments. Mind mapping has helped me to learn new ways to organize my thoughts, compare alternatives, plan, express myself, and remember a lot of the day by day tasks I want to continue to do for myself as long as possible.
Not everyone will use these techniques in the same way and I hope that anyone who tries gets to experience the feelings of “control over my own life” that I continue to feel.
Yes I need help but these techniques help me minimize the burden on caregivers and family and let me continue to enjoy my profession which was also my most enjoyable “hobby.”
This is among of the most helpful dementia resources I’ve found. It acknowledges and addresses the needs of the caregiver and sufferer (often neglected elsewhere) with unique clarity and empathy. Really remarkable!
I’ve shared it with a caregiver and a person suffering from dementia. I have high expectations that it’ll facilitate a much needed change in perspective and help to relieve suffering. There’s nothing more valuable.
Thank you Dorlee! Thank you Dr. Huba!
Rick,
Thanks so much for your kind and thoughtful feedback! I’m so glad that you found this interview with Dr. Huba such a helpful resource to share with both a caregiver and person suffering with dementia.
In all likelihood, how effective and helpful these resources will depend on how far along a person is with their dementia (as well as when they first started using these resources), how adept the caregiver becomes with mind mapping, and the specific mind mapping program used.
For example, when you look at my mind map from coggle (free version), it is much harder to read vs. Dr. Huba’s mind maps which are sharper/brighter and easier to read.
Thanks again! I will send an email to Dr. Huba to ensure he sees it 🙂
Best,
Dorlee
Thank you for your comments; greatly appreciated. I find that the method motivates me to engage with ideas and is a great way for me to organize them.
It is also fun which is something which is quite important, especially as one progresses into more advanced stages of dementia and more severe symptoms.
Please keep us informed of your progress in working with clients and exploring the techniques for your own use.
Many people diagnosed with dementia do not like the term “suffering with dementia” and prefer the term “person with dementia” or PWD because we think that you can live well with dementia with help and your own efforts.
I appreciate the purpose of the article and am wondering how anyone who has a cognitive decline of the sort mentioned, would also have the capacity and patience to follow along with the protocols stated in this article.
Hi Sherry,
Thank you for sharing your thoughts and questions.
I too would have never considered mind mapping as a possible helpful coping strategy for someone experiencing dementia prior to conducting this interview with Dr. Huba.
He himself states that the methods he employs are likely to help some individuals at the early to mid-stages of dementia.
However, isn’t the possibility that these methods may work even for some unknown percentage of individuals at the early to mid-stages exciting? (And they have and do for Dr. Huba!)
Please make sure to check out the wonderful ebook Mind Mapping, Cognitive Impairment, and Dementia he has authored with 500 mind maps on this very topic! 🙂
Best,
Dorlee
Thank you for your comment.
One of the things that seems to most frustrate those persons with dementia who blog (see the blog of Kate Swaffer as an excellent example) is that most people have difficulty understanding that sometimes when we cannot remember names or an appointment or to buy vegetables we can do very advanced things like write a cookbook and travel the globe speaking (Ms Swaffer) or write out equations from multivariate statistical procedures (me) but not be able to solve “word” math problems from a fourth grade text. Or still give drivers of the car I am in better instructions about how to go from point A to point B than they have figured out but be unable to assemble Lego projects designed for 10 year olds (I can still painfully put together those for 6 year olds).
I can tell you how to do your taxes and answer some pretty complex questions about the tax code for business while not being able to collect all of the forms and receipts needed to do my own tax return. I write a lot about this on my blog, Hubaisms.com. Many others do likewise on their blogs or in comments in social media.
If you could take a picture of my brain, I think it would look like one of those “Cheese Head” hats fans of the football Green Bay Packers wear. As I experience it, the pattern of “holes” in my brain is almost random and the fact that I cannot do something “simple” does not mean I cannot do something “hard.”
The neurological literature (important peer-reviewed journals) documents a number of cases where patients with (FTLD dementia) often experience bursts of creativity and express new cognitive skills, perhaps as a form of adaptive brain plasticity. Ravel is believed to have written Bolero — the highest royalty piece of classical music ever, an index of its popularity — after FTLD. I think that people with many other types of dementia may experience the same thing but because Alzheimer’s disease, for example, is not usually detected until quite advanced, is not as easily noticed.
And yes, after a day of thinking about how to reply to your comment, and about a dozen edits of these sentences, I can still write a reply like this. Just don’t ask me to give it to you in a conversation or understand your comment if you tell it to me in a social situation, especially if a radio is on or people are talking in the background. I probably could answer your question the next day after I remember my ideas, but I have an extremely hard time finding the right words to speak.
I’m a big “Cheese Head” from the old days, but I think football should be banned because I would never want anyone to have experience what I (and many former football players) experience.
Very interesting. I find so much variaton in abilities from client to client and I was wondering if you see certain mind mapping strategies work better with certain dementias. certain stages? Maybe this is covered in the book which I’m definately downloading. thanks…
Thanks so much for stopping by, LuAnn
I think I can partially respond to your question and I’ll have to leave the other part to Dr. Huba 🙂
Dr. Huba is reporting and sharing the results of his work on himself; this means that we know that the techniques he is sharing work for early to mid-stage of dementia. I’m not sure about what his particular type of neurodegeneration disorder he has but perhaps he can shed clarity about this when he responds (probably tomorrow).
How wonderful you decided to treat yourself to his book – it’s a real work of art and full of so many creative ideas!
Best,
Dorlee
Thank you for your questions. I am currently diagnosed as having FTLD (or FTD in earlier papers). This type of dementia, although relatively rare, is the most diagnosed among early onset cases of dementia. FTLD is diagnosed 10-15 years earlier than Alzheimer’s.
What works best with what type of dementia under certain conditions is a very difficult thing to answer as it would require many decades of empirical study and then at the end the academics would say we still don’t know.
I already have guidelines in many of my posts on Hubaisms.com but they are embedded within the topics. I am going to pull information from a lot of those posts plus additional materials and create a new series of posts to answer your questions specifically. Look for some guidelines on Hubaisms.com starting in April 2016.
Interesting idea! The fact that it is ‘expensive’ and requires hours of commitment is a concern though. Does the professional have the time to create the mind map and can the individual with dementia or cognitive decline fully participate in the process or is the family willing to participate if need be? What if there is no family or caregiver(s)? There are many individuals with cognitive decline that are alone either by circumstance or choice.
I will look into this more as I am curious about the mind map idea.
Thanks for this article Dorlee!
Hi Vikki,
Thanks so much for sharing your thoughts and questions.
I’ll share with you my thoughts and then I’ll alert Dr. Huba so that he may respond.
I agree with you that the mind mapping program that Dr. Huba recommends is rather expensive and requires a few hours of training to get up-to-speed; however, one can also try out less expensive or free mind mapping programs to see if they work with one’s clients. There is coggle (for example) which is free and this 1 minute tutorial demonstrates how easy it is to use.
If you find that mind mapping is indeed helpful for your clients/relatives with cognitive decline, you could then decide whether or not to invest in the top of the line variation with its bells and whistles.
Also, if you have a number of clients with dementia and you are able to illustrate the mind mapping benefits to your employers, is it possible that your agency may be willing to cover the mind mapping software expense?
With respect to the time question, in all likelihood the professional is already investing time to explain things to the individuals with dementia and/or their caregivers… and the individuals with dementia struggle to remember what it is the professional just shared with them. Now, they will have an engaging visual to jar their memory.
Making these mind maps together with the persons with dementia and/or their caregivers sounds like a wonderful way of further engaging both the patients and their caregivers in the process 🙂
What if there are no caregivers/family members? I would imagine that these mind maps would further facilitate people with dementia being able to live on their own a bit longer than otherwise.
Thanks again!
Best,
Dorlee
Thank you for the comments.
I do not really think that the cost for iMindMap is that much for what it does. After just a short period of time you will able to quickly draw bright, happy maps with it that will catch the attention of the PWD (person with dementia). I think that you probably can be making great maps of menus, to-do items, appointments and similar “social worker” applications after 2-4 hours of video watching. Or if you look at some of my examples you could copy them. I am very sure this program works better than anything else although there are many programs which cost more. Remember too that this should be a tax deductible professional tool in the USA (ask your accountant).
I would try the free trial and see what you think after watching 1-2 hours of basics. Can you draw basic maps and make them look compelling for a client. At the end of the trial if you think it is worth it, buy it and see what free videos are available and if you think it would be worth it to watch some.
Want something cheaper (but not free), MindNode PRO for the Mac (only) is somewhere in the $30-50 range.
If you want something good and relevant to start on before you try to the use program with a client, try making a few maps of case notes or your schedule or a lecture.
You can use this for a number of applications with any of the dyads or triads of you+PWD, you+caregiver, you+family, you+PWD+ caregiver, ETC. I think you might find this more useful in working one-on-one with a client and then explaining the map to the family and/or caregiver, or various combinations.
Hope this is helpful. The questions on Dorlee’s article have making some bells go off in my head, so I would expect to see posts that address the questions I am being asked within the next few weeks.
iPad versions of iMindMap and MindNode are also available at a much lower cost than a notebook version but I personally find them too small work with comfortably.
As for which clients to start with, I would experiment first with someone with young onset dementia who had a “computer related” job and is at an early stage in their dementia. That should be your easiest client for this kind of technology and a good place for you to hone your skills.