 Suicidal Ideation: 4 Documentation Tips
Suicidal Ideation: 4 Documentation Tips
What to Write When a Client Tells You They Are Contemplating Suicide
When a client expresses suicidal ideation i.e., a client tells you they no longer want to live and is able to describe how they would end their life, most counselors go into a place of both hyperfocus and multitasking. They zero in on what exactly is leading to the feelings, ask questions to complete a risk assessment, then create a plan with the client for how to move forward.
They do all this while simultaneously considering their options for how to address the client’s need and managing their own emotions that arise in this high stress situation. Once the situation has passed and the client is out of the office the counselor is then left to do the one thing they know is crucial but also increases their anxiety about the situation- write their case note.
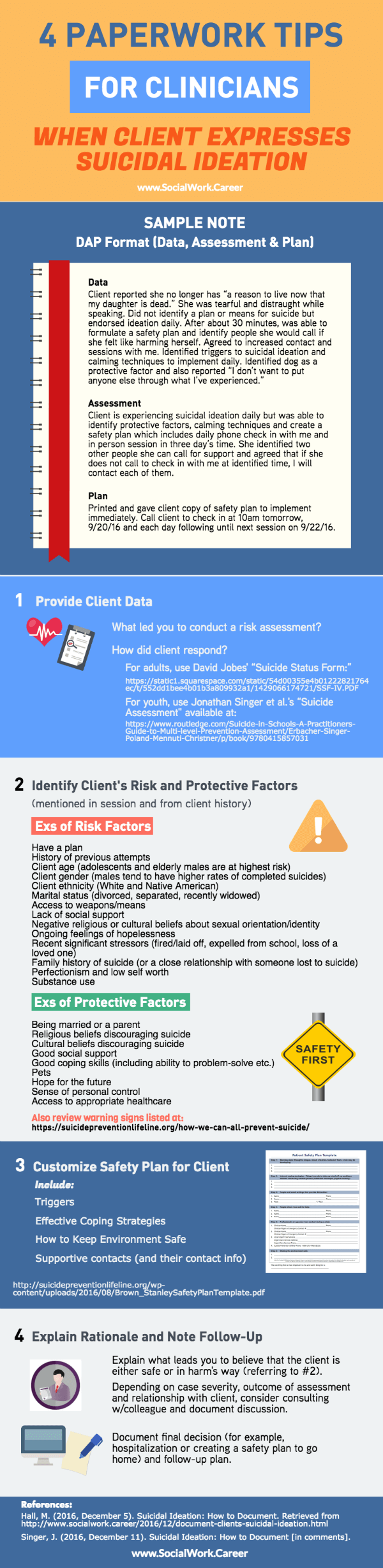
While no client or situation is the same, there are some general principles you can apply to the practice of writing these notes that will help you cover yourself ethically but also help you become a better clinician. Let’s look at four key components of good documentation after completing a suicide risk assessment:
Provide Client Data
In your note, clearly identify what led you to complete a risk assessment. Was it a clear quote from the client saying they wanted to harm themselves? Or was it something more subtle, like a passing statement they made about not wanting to be around any longer?
This information is key for explaining your rationale, which we’ll review further down. It is important to highlight exactly what it was that caused the initial concern and then to review how the client responded after you began seeking more information. A general guide you can use is that if the client mentioned or did something that made you seek further information, that’s something you want to include in your note.
Identify Risk and Protective Factors
Suicide research provides us with many factors that contribute to suicide attempts. Not only do you want to consider these factors in your actual assessment, you want to include them in your note. List everything you identified in your session, as well as factors of which you’re aware from previous sessions or client history.
Perhaps the client reported having a plan, was recently widowed and has a distant relationship with his children. These are three indications that lead to a very high risk situation and would serve as support for your seeking hospitalization with your client, if further details were also provided.
Here are other risk factors that tend to be correlated with higher risk of suicide that you can include in your note, if applicable (see references below):
-
History of previous attempts (this is the most correlated with risk of future attempts)
-
Client age (adolescents and elderly males are at highest risk)
-
Client gender (males tend to have higher rates of completed suicides)
-
Client ethnicity (White and Native American)
-
Marital status (divorced, separated, recently widowed)
-
Access to weapons/means
-
Lack of social support
-
Negative religious or cultural beliefs about sexual orientation/identity
-
Ongoing feelings of hopelessness
-
Recent significant stressors (fired/laid off, expelled from school, loss of a loved one)
-
Family history of suicide (or a close relationship with someone lost to suicide)
-
Perfectionism and low self worth
-
Substance use
Likewise, it is just as important to document protective factors that may play into your decision. Even people with a history of hopelessness and little social support will often identify their pets as a reason they would never fully act upon any ideation. This would be a great protective factor to identify in your note, particularly if you can quote the client saying something like “but I would never do that because there is no one to take care of Buster.”
Here are some protective factors you may want to consider in your assessment and include in your note (see references below):
-
Being married or a parent
-
Religious beliefs discouraging suicide
-
Cultural beliefs discouraging suicide
-
Good social support
-
Good coping skills, ability to problem-solve and history of managing behaviors
-
Pets
-
Hope for the future
-
Sense of personal control
-
Access to appropriate healthcare
It is important to note here that the purpose of documenting risk and protective factors is to support your decision, along with other evidence and a more detailed rationale. Identifying risk and protective factors alone does not suffice for a personalized assessment.
Write a Safety Plan, Not a Contract
Research (see references below) has led us to shift from creating “No Harm Contracts” or “Safety Contracts” to Safety Plans. The reason? There was no evidence to support that contracts either reduced suicide attempts or reduced clinician liability when clients attempted suicide. The major shift in thinking here was from liability protection to client resilience and support.
A Safety Plan is not an agreement to avoid something; instead, it provides tools and resources for the client and ways in which they can act when experiencing feelings or urges.
Some things to include in a Safety Plan may be:
-
Triggers that tend to lead to feelings of hopelessness or self-loathing
-
Proven coping skills that have been practiced in session
-
Ways in which to keep the environment safe
-
People who can provide support, along with contact information for those people
This is certainly something that is developed in collaboration with the client, rather than a contract presented to sign. Each Safety Plan would look very different for each client, as it focuses on what helps get through difficult days.
Another benefit to the Safety Plan is that you can use this prior to expressed suicidal ideation. Use it as a prevention strategy and document any time you have created, discussed or modified the Safety Plan.
Explain Your Rationale
You know your client so take that into consideration. However, explain in your note why that impacts your decision. Consider your note as if you were doing a consultation with another professional and explaining to them what is leading to your confidence that the client is either safe or in harm.
Go back to your risk and protective factors, the client’s triggers and red flags. Why does one potentially outweigh the other?
For example, a client may say they are hopeless, no longer want to live and have no reason for being anymore. They have identified a vague plan for how to end their life but not for how to ensure their pet is cared for if they enacted the plan. They have never attempted suicide in the past and also report a strong religious belief that “I will go to hell if I go through with it and then I’ll never see my husband again, anyway.”
These things together provide a great summary of the client information that led to your decision. Then document what the final decision was (for example, hospitalization or creating a safety plan to go home) and how you plan to move forward. Include anything that may have impacted your decision- environmental factors, history, client behavior, etc.
Sample Note
Interested to see what this all looks like in (semi) real life? Here’s an example of a note for an imaginary client who expressed suicidal thoughts but was able to create a safety plan. This note uses the DAP (Data, Assessment, Plan) format:
Data: Client reported she no longer has “a reason to live now that my daughter is dead.” She was tearful and distraught while speaking. Did not identify a plan or means for suicide but endorsed ideation daily. After about 30 minutes, was able to formulate a safety plan and identify people she would call if she felt like harming herself. Agreed to increased contact and sessions with me. Identified triggers to suicidal ideation and calming techniques to implement daily. Identified dog as a protective factor and also reported “I don’t want to put anyone else through what I’ve experienced.”
Assessment: Client is experiencing suicidal ideation daily but was able to identify protective factors, calming techniques and create a safety plan which includes daily phone check in with me and in person session in three day’s time. She identified two other people she can call for support and agreed that if she does not call to check in with me at identified time, I will contact each of them.
Plan: Printed and gave client copy of safety plan to implement immediately. Client will call to check in at 10am tomorrow, 9/20/16 and each day following until next session on 9/22/16.
If you use any formalized assessment tool as an aide in your process such as David Jobes’ “Suicide Status Form” for adults or Jonathan Singer et al.’s assessment for youth, you’ll want to include that in the client file and reference it in your note, as well.
Also include a copy of the safety plan you create with the client. If the safety plan is included in your file, then you do not need to add all the details of the safety plan in your note and can eliminate some redundancy.
What’s Next?
I would be remiss if I didn’t remind you that beyond documenting the risk assessment, the second most important thing is documenting your follow-up. Make sure you identify a clear plan moving forward (separate, but in addition to the Safety Plan created with the client) and then clearly explain that follow up.
As someone who has reviewed hundreds of client files, I can say this is one of the biggest missing pieces. Many clinicians are wonderful at documenting the crisis but then, a week later, it’s as though nothing ever happened.
Continue to document ongoing assessment, check-ins, and consultation with other providers. This closes the gap and completes the story.
Although risk assessments and crisis situations can be stressful, there is no reason your documentation should cause more stress. Use your notes as a way to process the situation and plan ahead to make sure you have the necessary time. That way you can feel confident you have done your best to help in every way possible.
Like this post? Please share it!
References:
https://wmich.edu/suicideprevention/basics/protective
http://www.sprc.org/sites/default/files/migrate/library/RiskProtectiveFactorsPrimer.pdf
http://www.cdc.gov/violenceprevention/suicide/riskprotectivefactors.html
http://www2.isu.edu/irh/projects/better_todays/B2T2VirtualPacket/SuicidePrevention/SAFETY%20PLANS%20for%20Suicide%20Prevention%20final%20pdf.pdf
http://www.speakingofsuicide.com/2013/05/15/no-suicide-contracts/
About the Author: Maelisa Hall, Psy.D. specializes in teaching therapists how to connect with their paperwork so it’s more simple and more meaningful. The result? Rock solid documentation every therapist can be proud of! Check out her free online Private Practice Paperwork Crash Course, and get tips on improving your documentation today.

Thank you for this quick and easy guide to documenting suicide risk. Dr. Hall covers many best practices for documenting a suicide assessment. Her recommendation to use the Safety Plan is spot on. I would like to punctuate a few points:
1. Dr. Hall is correct when she says to write down WHY you conducted a suicide risk assessment. Dr. Hall writes, “A general guide you can use is that if the client mentioned or did something that made you seek further information, that’s something you want to include in your note.” Just to clarify, what you include is your client’s exact words. Dr. Hall demonstrated this in her sample note when she quoted the client as saying “I don’t want to put anyone else through what I’ve experienced.” Using your client’s actual words in quotes is counter to the advice for most clinical documentation. But there is a big difference between the quote Dr. Hall included in the note, and writing “client reported not wanting to put anyone else through this.”
2. Dr. Hall is correct that it is important that you’ve assessed for risk factors. The key statement in her review is “Identifying risk and protective factors alone does not suffice for a personalized assessment.” The reason they don’t suffice is that Risk factors for suicide are characteristics that are present more often in people who have died by suicide than people who have not died by suicide. The list of risk factors Dr. Hall provides might not have anything to do with your client. Dr. Hall is right that history of previous attempt, age, ethnicity, gender, access to guns, etc are all risk factors. But they might be present in your client and not be associated with imminent risk. The things that are specific to your client are called “warning signs.” Warning signs are those things that indicate risk for imminent harm for your client such as talking about wanting to die or to kill themselves or looking for a way to kill themselves, like searching online or buying a gun. The National Suicide Prevention Lifeline has a nice summary of risk factors and warning signs: https://suicidepreventionlifeline.org/how-we-can-all-prevent-suicide/
3. A similar point needs to be made about protective factors. First, I’ll say that Dr. Hall’s list of protective factors is accurate. But, documenting protective factors without pairing them with a specific risk does nothing for your liability nor for your client’s safety. The reason marriage is a protective factor is that married people are statistically less likely to die by suicide than single people. But, that might not apply to your client. If it is a “protective factor” for your client you need to clarify what specific risk it protects against. If the risk is isolation, then being in a loving marriage might protect against isolation. If so, you need to clarify that in your documentation. For the sample progress note this would look like, “Identified dog as a protective factor *because ‘the dog gives me a reason to live. As sad as I get, I’d never leave that dog.'”
4. In the documentation the clinician writes that the client will follow up the next morning. I would advise clinicians to document that THEY will follow up with client the next morning. This isn’t so much about how to document as it is to make sure you’re documenting best practices. For my non-suicidal clients it is totally reasonable to expect that they will follow up with me.
5. Under “Explain Your Rationale” Dr. Hall writes, “Consider your note as if you were doing a consultation with another professional…” I would add that you should actually consult with another professional and document that consultation when doing a suicide risk assessment. Dr. Hall mentions this under “What’s Next,” but I would encourage you to consult “Right Now.” You could also imagine that your notes have been subpoenaed and are being read by a judge with NO training in mental health. Have you walked her through your thought process? If not, revise your documentation.
6. If you are doing a suicide assessment, your note should be longer and more detailed than the one provided by Dr. Hall. If you don’t have a document that walks you through a suicide assessment, get one. My coauthors and I created one for our book “Suicide in Schools.” You can find the suicide assessment at the publisher’s website under eResources > Risk Assessment Resources: https://www.routledge.com/Suicide-in-Schools-A-Practitioners-Guide-to-Multi-level-Prevention-Assessment/Erbacher-Singer-Poland-Mennuti-Christner/p/book/9780415857031
Thank you so much, Jonathan/Dr. Singer, for providing your detailed feedback and commentary on Maelisa’s post.
Your expertise in the suicide prevention arena comes through loud and clear, and I look forward to reading the book you’ve co-authored on the subject!
My readers and I most appreciate being able to learn from you both! And as I’m thinking about it, Maeilisa may wish to incorporate some of these learnings into the post, and similarly, I think I’d like to update the infographic accordingly.
I love the suicide assessment form that you and your co-authors provide as a free resource. Do you happen to have a variation that you recommend for adults?
With much appreciation and warm regards,
Dorlee
Jonathan,
Thanks so much for sharing these additional resources! This is excellent. Thanks also for adding some further comments to the blog post. This is such an important and BIG topic; any additional feedback is appreciated.
Please note we did take some of this great info and added to the post.
I would caution clinicians to focus on length of notes only. Content is really king in the world of notes, as many looooong notes can still miss the mark when it comes to the necessary info. That’s why it is so great you have an assessment tool that people can incorporate into their client file.
Thanks again for all your support!
Maelisa
Maelisa,
Thank you for starting the conversation. It is VERY important. Regarding the length of the note, you’re absolutely right – a long note isn’t necessarily a good note.
Best regards,
Jonathan
Dorlee,
Happy to contribute to this amazing resource you’ve created.
The form we developed could be used with adults, but a better form would be David Jobes’s “Suicide Status Form.” He developed the SSF as part of his Collaborative Assessment and Management of Suicidality (CAMS) model. You can find a PDF version here: https://static1.squarespace.com/static/54d00355e4b01222821764ec/t/552dd1bee4b01b3a809932a1/1429066174721/SSF-IV.PDF. You can read a peer-reviewed journal article about the SSF here: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3752846/. You can learn more about CAMS here: http://cams-care.com/cams/
I hope you find my book useful.
Best regards,
Jonathan
Thanks so much, Jonathan! It is thanks to Maelisa’s wonderful post, and soon also your contributions!
You obtain more information from David Jobe’s “Suicide Status Form” than the typical suicide assessment forms/methods, and thus gain a more accurate picture… I also like the tools it gives you to use in subsequent sessions to monitor the patient’s feelings.
I also look forward to reading the materials you’ve linked to support/explain further the CAMS model.
Re your book on Suicidality in Schools, there is no doubt that I will find it useful. Please keep some space in your calendar for a subsequent interview!
With much appreciation and best regards,
Dorlee